Colour Doppler ultrasound: application in cardiological diagnosis
Colour Doppler echocardiography or colour Doppler ultrasound is an indispensable diagnostic tool in cardiology.
Introduction
Echocardiography is considered the technique of choice for assessing cardiac structure and function.1 There have been numerous technological advances between the earliest M-mode ultrasounds conducted in human medicine in the 1950s and today’s 4D echocardiography, and some have meant that these techniques are increasingly accessible, not only to cardiologists, but also to general veterinary surgeons with an interest in ultrasound as a diagnostic tool.
Colour Doppler ultrasound has been used in veterinary medicine since 1986, although back then it was beyond the reach of most. In 1998, it was described as “a sophisticated form of ultrasound technology that overlays blood flow and velocity information onto a B-mode, two-dimensional, grey-scale image”.2 To ensure the technique is employed correctly, it is important to know how it works and its applications in veterinary cardiology.
Colour Doppler ultrasound: principles
Colour Doppler ultrasound is governed by the same basic principles as other ultrasound techniques, that is, high-frequency sound waves are emitted by piezoelectric crystals housed in the transducer and then travel through the internal structures of the organism and, following interaction with the tissues, are reflected back to the transducer, where microprocessors transform the information received into a moving image.1
Doppler ultrasound has some different properties lacking in M-mode and two-dimensional ultrasound. These characteristics are based on the work of Christian Andreas Doppler, an Austrian mathematician and physicist. In the 19th century, Doppler discovered that the wavelength of sound waves changes when the point of wave emission is moving relative to the point of reception. As we move toward the source of emission of the wave, its tone or frequency increases; conversely, it decreases as we move away. This change between the frequency of emitted and received sound is known as the Doppler effect.
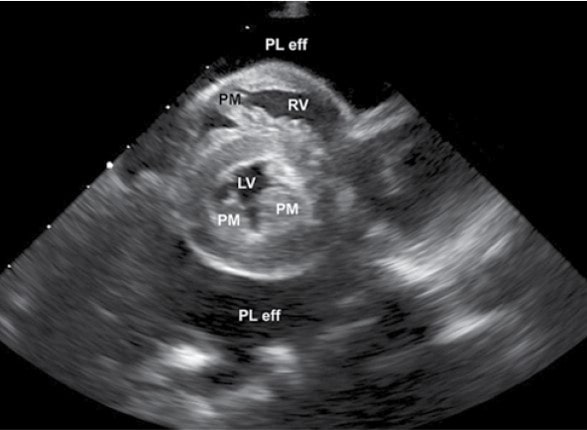
Extrapolating the idea to Doppler ultrasound imaging, there is a static source of ultrasounds (the probe) and mobile points of reception (blood cells inside vessels or the heart chambers) either moving towards or away from the probe.3 Given the emitted frequency, received frequency, speed of propagation of the sound and angle of incidence, the software that comes with ultrasound equipment estimates the velocity, direction and characteristics of the blood flow.
This information is displayed on a colour-coded map, where red is generally used for the flow toward the probe and blue for the flow away from it, while a lack of flow is shown in black. Within this range of colours, lighter tones are associated with higher velocities, while darker tones indicate slower flows. This is called a BART map (blue away, red towards), but most devices offer a range of colour-coded maps, so the technician can select the most appropriate for each case.
Colour Doppler ultrasound is a type of pulsed Doppler, which means the technician can choose the point at which to analyse the flow, although there are limitations as to the maximum velocities that can be detected with precision. When this limit is reached, the flow rate and direction are not represented correctly and the colours merge in a mosaic pattern, known as aliasing. This can indicate turbulent blood flow due to disease, but it can also occur when there is laminar flow if the probe frequency is set too high. In these cases, the colour scale can be adjusted by moving the 0 in either direction to increase the maximum measuring speed, or a lower frequency probe can be used, if available, to check whether or not the turbulence remains.
Colour Doppler ultrasound: uses
Colour Doppler ultrasound can be used to investigate the presence and direction of blood flow in various anatomical regions and provide data at diverse points of the cardiac cycle. It also a very quick method for exploring different areas of the heart walls and atrioventricular septum in search of possible defects.2
Therefore, it is an essential technique when assessing patients with suspected congenital heart disease and can also be very useful during the examination of many acquired heart diseases. Lastly, colour Doppler ultrasound has also been applied in myocardial motion analysis (tissue Doppler) to study the myocardium’s systolic and diastolic function.3,4
Either way, the correct interpretation of colour Doppler ultrasound involves studying the electrocardiogram tracing and B-mode image simultaneously, as well as knowledge of cardiac pathophysiology.
Conclusions
Colour Doppler ultrasound is a very useful tool for the diagnosis of many heart diseases. It is a quick, noninvasive method for assessing blood flow properties during the cardiac cycle. However, it is important to be aware of its limitations and interpret the results alongside the rest of the echocardiogram, clinical picture and the results of other diagnostic tests.